
Do I qualify for a special enrollment period?
You may qualify for a Special Enrollment Period if you or anyone in your household lost qualifying health coverage in the past 60 days (or more than 60 days ago but since January 1, 2020) OR expects to lose coverage in the next 60 days.
How does the Special Enrollment Period work?
Special enrollment in Maryland
- You qualify for a special enrollment period if you have a certain life event.
- You generally have 60 days from the date of your qualifying life event to enroll for health coverage or change your plan.
- In most cases, you need to have proof of your life event.
When is your Medicare supplement special enrollment period?
Your Special Enrollment Period starts 60 days before and lasts for 63 days after your previous coverage ends. Your Medicare Supplement policy can’t begin until your previous coverage is fully cancelled. Issues with Your Medicare Advantage Policy?
How to qualify for a special enrollment period under ACA?
You qualify for a Special Enrollment Period if you’ve had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child. Depending on your Special Enrollment Period type, you may have 60 days before or 60 days following the event to enroll in a plan.
What is Medicare special enrollment period?
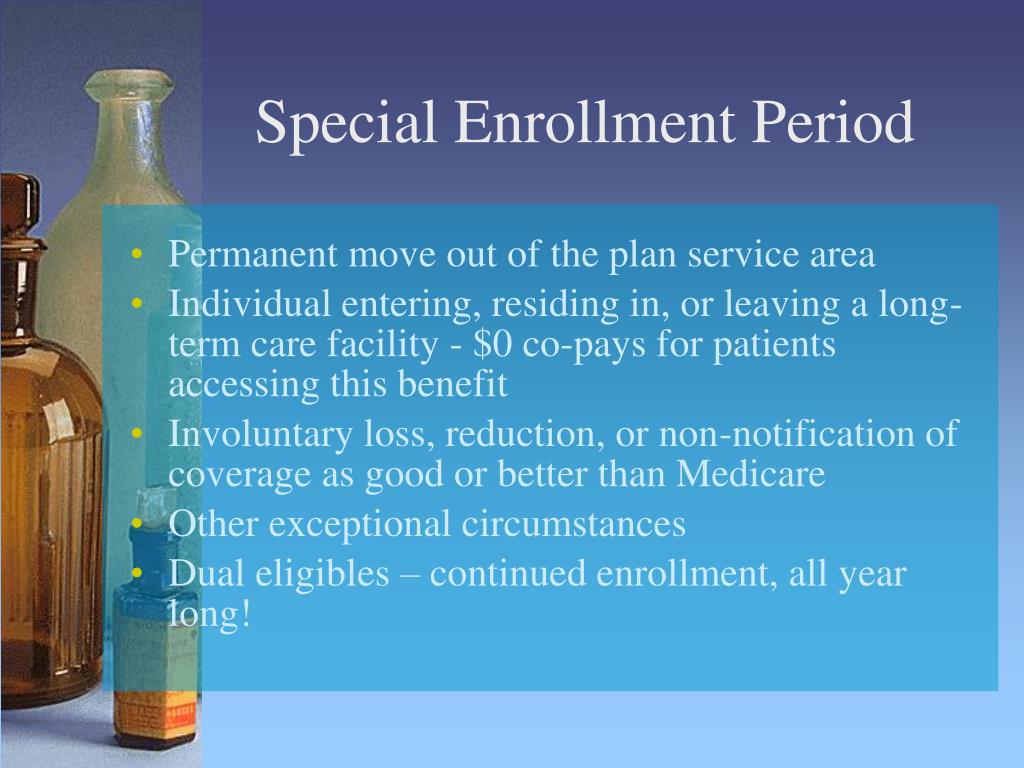
You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is the meaning of enrollment period?
Period of enrollment. Period of enrollment means the period that the title IV institution has established for which institutional charges are generally assessed (i.e., length of the student's course, program, or academic year.)
How long is the special enrollment period for Medicare Part B?
It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65. My birthday is on the first of the month. If you miss your 7-month Initial Enrollment Period, you may have to wait to sign up and pay a monthly late enrollment penalty for as long as you have Part B coverage.
What does enrollment period mean in insurance?
The yearly period in the fall when people can enroll in a health insurance plan for the next calendar year. Open Enrollment for 2022 is over, but you may still be able to enroll in a Marketplace health insurance plan for 2022 if you qualify for a Special Enrollment Period.
Why do enrollment periods exist?
Why do we have an open enrollment period? The open enrollment period was put into place to discourage adverse selection – which happens when sick people sign up for health insurance and healthy people don't. It greatly skews the amount of financial risk a health plan takes when insuring customers.
What enrollment means?
Enrollment is the act of enrolling at an institution or in a class. A fee is charged for each year of study and is payable at enrollment. Synonyms: enlistment, admission, acceptance, engagement More Synonyms of enrollment. 2. uncountable noun.
How do I get my $144 back from Medicare?
Even though you're paying less for the monthly premium, you don't technically get money back. Instead, you just pay the reduced amount and are saving the amount you'd normally pay. If your premium comes out of your Social Security check, your payment will reflect the lower amount.
Can you add Medicare Part B at any time?
If you did not enroll for Part B during your initial enrollment period, you may qualify for a Special Enrollment Period (SEP) to sign up for Part B (and/or Part A) anytime as long as you or a spouse is working and you're covered by a group health plan through that employment.
What are the Medicare Part B premiums for 2022?
The standard monthly premium for Medicare Part B enrollees will be $164.90 for 2023, a decrease of $5.20 from $170.10 in 2022.
How do I enroll in insurance after open enrollment?
If you're looking to enroll in a health insurance plan after the open enrollment deadline, here are a few options:Marketplace Special Enrollment Period. ... Medicare Special Enrollment Periods. ... Medicaid or CHIP. ... Short-term health insurance plans. ... Supplemental health insurance.
What is the difference between open enrollment period and annual enrollment period?
Medicare Annual Enrollment is when anyone who has Medicare can make coverage changes for the upcoming year, while Medicare Advantage Open Enrollment is only for people who are currently enrolled in a Medicare Advantage plan.
What is a qualifying event for insurance?
Qualifying life events typically include, but are not limited to: Becoming newly married or divorced. Having a baby or adopting a child. Experiencing a death of the insurer in the family. Losing health insurance coverage due to job loss.
What does time period currently enrolled?
Currently enrolled means the student has a course status of enrolled and is studying in the current teaching period or; the student has status of inactive and has r‐enrolled in a teaching period yet to commence (i.e. between teaching periods).
What is the difference between open enrollment period and annual enrollment period?
Medicare Annual Enrollment is when anyone who has Medicare can make coverage changes for the upcoming year, while Medicare Advantage Open Enrollment is only for people who are currently enrolled in a Medicare Advantage plan.
What is meant by open enrollment?
: a period of time during which you can join something as a member or participant : a period of time during which you can enroll in something. Employees can sign up for new benefits during open enrollment.
What is the meaning of date of Enrolment in Indian army form?
Date of enrollment means the date on which the applicant was approved as.
When does the enrollment period start for a group health plan?
Your initial enrollment period starts three months before the month you attain age 65 and ends three months after the month you turn 65. If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months.
What is a SEP in health insurance?
You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.
Do people on Social Security have a special enrollment period?
People who receive Social Security disability benefits and are covered under a group health plan from either their own or a family member's current employment also have a special enrollment period and premium rights similar to those for workers age 65 or older.
What is a special enrollment period?
A special enrollment period is a time when you’re allowed to make changes to your health insurance plan even though it’s not an open enrollment period as defined by the Affordable Care Act (ACA).
How do I know if I qualify for a special enrollment period?
In order to qualify for a special enrollment period, you need to have a qualifying life event happen that would cause needed changes to be made to your health coverage.
How to check if you qualify for a life event?
If you’ve experienced a qualifying life event, you can apply online. You can check to see if your life event qualifies by going to Healthcare.gov and answering a few screening questions to see if you qualify for a special enrollment period.
How long do you have to enroll in a new health plan?
Generally speaking, you’ll have 60 days following the event to enroll in a new health plan through the federal or state marketplace. Keep in mind, you’re eligible to enroll in Medicaid or the Children’s Health Insurance Program (CHIP) at any time.
Can you change your health insurance if you have a qualifying life event?
Having a qualifying life event isn’t the only way you can qualify for a special enrollment period. Other circumstances that can allow you to make changes to your health coverage include experiencing an enrollment or policy information display error, gaining or becoming a dependent due to a child-support, or getting an appeal decision that’s in your favor.
What are the conditions for a special enrollment period?
Other life circumstances that may qualify you for a Special Enrollment Period: Gaining membership in a federally recognized tribe or status as an Alaska Native Claims Settlement Act (ANCSA) Corporation shareholder. Becoming newly eligible for Marketplace coverage because you became a U.S. citizen.
How long do you have to be in your household to qualify for special enrollment?
You may qualify for a Special Enrollment Period if you or anyone in your household in the past 60 days:
Can you enroll in a special enrollment period if you are moving?
Note: Moving only for medical treatment or staying somewhere for vacation doesn’t qualify you for a Special Enrollment Period.
Can you qualify for a special enrollment period if you lose Medicaid?
You may qualify for a Special Enrollment Period if you lose Medicaid or Children’s Health Insurance Program (CHIP) coverage because:
Can you appeal a decision to deny you a special enrollment period?
You can appeal the decision. Learn how to appeal the decision to deny you a Special Enrollment Period.
Can you get special enrollment if you lose health insurance?
You may qualify for a Special Enrollment Period if you lose health coverage through your employer or the employer of a family member, including if you lose health coverage through a parent or guardian because you're no longer a dependent.
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How long does Medicare Advantage coverage last?
If you had a Medicare Advantage plan with prescription drug coverage which met Medicare’s standards of “creditable” coverage and you were to lose that coverage through no fault of your own, you may enroll in a new Medicare Advantage plan with creditable drug coverage beginning the month you received notice of your coverage change and lasting for two months after the loss of coverage (or two months after receiving the notice, whichever is later).
How long do you have to disenroll from Medicare?
If you wish to disenroll from employer or union-sponsored coverage (including a group-sponsored Medicare Advantage plan) in order to enroll in Medicare Advantage, or you wish to disenroll from Medicare Advantage in order to join an employer or union-sponsored plan, you may do so for up to two months following the end of your previous coverage.
How many stars do you need to be to enroll in Medicare Advantage?
If you are enrolled in a Medicare Advantage plan that has received a Plan Performance Rating of three stars or less for three consecutive years, 1 you may enroll in a higher rated plan throughout the year.
What is the number to call for Medicare enrollment?
If you have a particular situation that prevented you from enrolling in any type of Medicare coverage for which you were eligible, you are encouraged to call 1-800-MEDICARE and request a Special Enrollment Period.
When does the initial enrollment period end?
Initial Enrollment Period (IEP) One Medicare enrollment period is the Initial Enrollment Period. The IEP allows you to sign up for Parts B and D when you turn 65. Your Initial Enrollment Period begins three months before the month you turn 65, includes your birthday month and ends three months after you turn 65.
What is the IEP2 enrollment period?
Initial Enrollment Period 2 (IEP2) Another enrollment period that is also 7-months is the Initial Enrollment Period 2. The IEP2 is for people who were already eligible for Part A and B before they turned 65. During the IEP2, you can sign up for a Medicare Advantage or Part D plan. The IEP2 runs for the same seven-month period as the IEP.
What is the ICEP period?
The ICEP is your first opportunity to choose a Medicare Advantage plan instead of Original Medicare. During the ICEP, you can also sign up for prescription drug coverage. If you enroll in Part B when you turn 65, your ICEP is the same as your IEP.
Why is Medicare enrollment confusing?
Medicare Enrollment Periods can be confusing because different enrollment periods have different dates for various purposes. There are many enrollment periods for people signing up for benefits for the first time. If you’re receiving Social Security or Railroad Retirement benefits when you turn 65, you’ll automatically be enrolled in Medicare.
What is open enrollment for Medicare 2021?
These enrollment periods fall into two categories. First, open enrollment is available to anyone eligible for Medicare. Then, Special Enrollment Periods. If you want to change the coverage you currently have, you can do so during one ...
How many enrollment periods are there for Medicare?
There are three enrollment periods for people signing up for benefits who are already enrolled in Original Medicare. During open enrollment, you can make changes to your Medicare plans and add additional coverage.
How long does an IEP2 last?
During the IEP2, you can sign up for a Medicare Advantage or Part D plan. The IEP2 runs for the same seven-month period as the IEP.