Does Medicare Advantage have benefit periods?
The Medicare Advantage plans that use benefit periods are typically for skilled nursing facility stays. A large majority of Medicare Advantage plans do not use benefit periods for hospital stays. Most beneficiaries pay a copayment for the first few days. Afterward, you’re required to pay the full amount for each day.
How does Medicare benefit periods work?
What Are Medicare Benefit Periods?
- Medicare benefit periods usually involve Part A (hospital care).
- A period begins with an inpatient stay and ends after you’ve been out of the facility for at least 60 days.
- You’ll pay different amounts based on how long you’ve been staying at an inpatient facility or facilities.
What benefits are covered by Medicare?
Medicare provides benefits for:
- consultation fees for doctors, including specialists;
- tests and examinations by doctors needed to treat illnesses, such as x-rays and pathology tests;
- eye tests performed by optometrists;
- most surgical and other therapeutic procedures performed by doctors;
- some surgical procedures performed by approved dentists;
What is the wellness period for Medicare?
for longer than 12 months, you can get a yearly “Wellness” visit once every 12 months to develop or update a personalized prevention plan to help prevent disease and disability, based on your current health and risk factors. The yearly “Wellness” visit isn’t a physical exam.
See more

How does Medicare benefit period work?
A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins.
Is a Medicare benefit period one year?
Medicare Part A covers an unlimited number of benefit periods, and it helps pay for up to 90 days of care for each one. After 90 days, it's possible to tap into lifetime reserve days.
What is meant by benefit period?
What Is a Benefit Period? A benefit period is the length of time during which an insurance policyholder or their dependents may file and receive payment for a covered event. All insurance plans will include a benefit period, which can vary based on policy type, insurance provider, and policy premium.
Can my Medicare benefits run out?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What happens when Medicare hospital days run out?
Medicare will stop paying for your inpatient-related hospital costs (such as room and board) if you run out of days during your benefit period. To be eligible for a new benefit period, and additional days of inpatient coverage, you must remain out of the hospital or SNF for 60 days in a row.
What is the 3 day rule for Medicare?
To qualify for Skilled Nursing Facility (SNF) extended care services coverage, Medicare patients must meet the 3-day rule before SNF admission. The 3-day rule requires the patient have a medically necessary 3-consecutive-day inpatient hospital stay.
Do Medicare days reset every year?
Does Medicare Run on a Calendar Year? Yes, Medicare's deductible resets every calendar year on January 1st.
What is the 60 day rule for Medicare?
If your break in skilled care lasts for at least 60 days in a row, this ends your current benefit period and renews your SNF benefits. This means that the maximum coverage available would be up to 100 days of SNF benefits.
What is maximum benefit period?
Maximum Benefit Period means that maximum amount of time, during which benefits will be paid under the Plan for your Non-Occupational Disability or Occupational Disability following the Elimination Period for the coverage you elected under the Plan as set forth in Appendix A.
Does Medicare cover 100 percent of hospital bills?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
What is the Medicare 90 day rule?
Original Medicare covers up to 90 days of inpatient hospital care each benefit period. You also have an additional 60 days of coverage, called lifetime reserve days. These 60 days can be used only once, and you will pay a coinsurance for each one ($778 per day in 2022).
Is there a maximum that Medicare will pay?
There is no limit to your potential medical bills under Original Medicare. Under current rules, there is no Medicare out of pocket maximum; if you have a chronic health condition or an unexpected health crisis, you could pay thousands in medical costs.
What is the difference between calendar year and benefit year?
A plan on a calendar year runs from January 1–December 31. Items like deductible, maximum out-of-pocket expense, etc. will reset every January 1. All Individual and Family plans are on a calendar year. A plan on a contract year (also called benefit year) runs for any 12-month period within the year.
How long is a benefit period for major medical expense plan?
one to three yearsA period of time typically one to three years during which major medical benefits are paid after the deductible is satisfied. When the benefit period ends, the insured must then satisfy a new deductible in order to establish a new benefit period.
What is the difference between plan year and calendar year?
The calendar year is January 1 to December 31. That's simple enough. A plan year is the 12-month period during which your health plan is effective. It is determined by your employer's group coverage start and end dates.
What month do Medicare benefits begin?
If you qualify for Premium-free Part A: Your Part A coverage starts the month you turn 65. (If your birthday is on the first of the month, coverage starts the month before you turn 65.)
Guide to Explaining The Medicare Hospital Benefit Period
Under Medicare, the hospital benefit period starts once you’ve been admitted to the hospital and expires once you’ve been at home for 60 consecutiv...
Traditional Medicare Hospital Coverage
Here is a breakdown of how much Medicare will cover and how much you’ll owe out-of-pocket for individual hospital benefit periods: 1. You will be e...
Skilled Nursing With Traditional Medicare Coverage
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a ho...
Options With Medicare Advantage
You are subject to Medicare’s hospital benefit periods if you have a Medicare Advantage health plan. However, the costs for skilled nursing and hos...
How long is a Medicare benefit period?
Medicare defines a benefit period as: A hospital stay of any length, Plus any time you spend recovering in an inpatient rehabilitation facility , Plus the 60 consecutive days immediately following your release. Benefit Periods Can Be Longer or Shorter Than Illnesses: The term “benefit period” only determines how you get billed.
When does the Medicare benefit period start?
Benefit Period Start: A Medicare benefit period will begin the first day you are admitted to a hospital. Emergency room visits don’t count unless you are admitted to the hospital directly from the ER. When you are first admitted to a hospital, you will have to pay your Medicare Part A deductible, which is $1,484 in 2021.
How much is Medicare Part A deductible for 2021?
When you are first admitted to a hospital, you will have to pay your Medicare Part A deductible, which is $1,484 in 2021. Most popular Medicare Supplements will cover this cost for you. Benefit Period End: Your benefit period will officially end 60 consecutive days after your release from the hospital or from rehab if there are no additional stays.
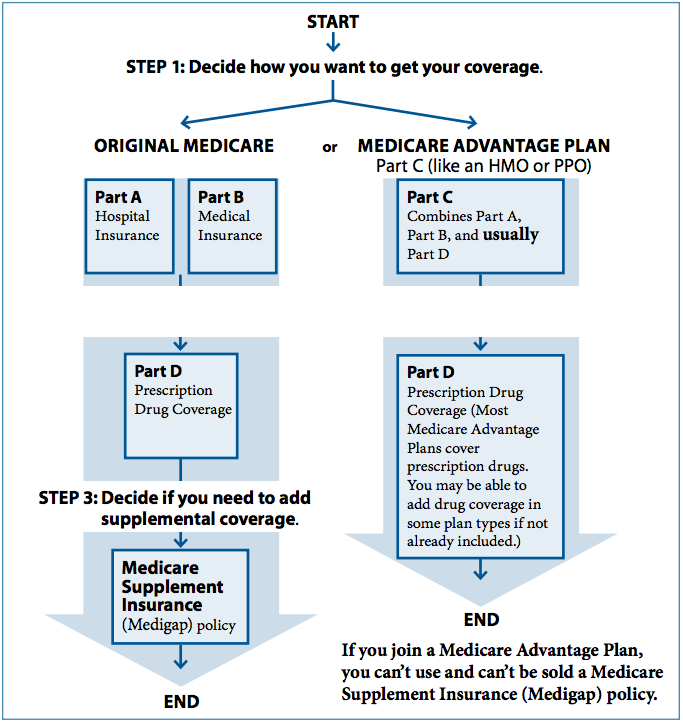
What is Medicare Advantage?
Medicare Advantage: Medicare Advantage, also known as Part C, plans replace your standard Medicare Part A and Part B. Your copayments would depend on the specific policy you chose. When hospital bills come knocking, Original Medicare (Part A and Part B) begins to show its flaws.
How many times can you pay your Part A deductible?
Worst case, that means you could pay your Part A deductible up to five times in a calendar year – in addition to your regular ...
Is Original Medicare enough?
Many people find that having Original Medicare is not enough to shield them from big deductibles and copayments, like the two scenarios at the beginning of this article. If you feel the same way, then take the time to explore your extra coverage options on HealthCare.com.
Is a benefit period longer or shorter than an illness?
Benefit Periods Can Be Longer or Shorter Than Illnesses: The term “benefit period” only determines how you get billed. It does not mean the length of an illness or the length of time you are treated for a condition. That’s important to know.
What happens after 90 days of Medicare?
After day 90 in a benefit period, and if the person has no more lifetime reserve days available to use, the Medicare recipient is responsible to pay all of the costs associated with their hospital stay. After you’ve spent 60 days out of the hospital, your benefit period will start all over again. At the start of each new period, you will receive ...
How many days do you have to be out of the hospital to get Medicare?
In order to help you make better sense of this, here’s a breakdown. 60 days: How many days you are required to be out of the hospital or after-care facility to become eligible for another hospital benefit period. 60 days: The maximum number of days that Medicare will pay for all of your inpatient hospital care once you’ve paid your deductible ...
What if I use up all my lifetime reserve days but need more coverage?
And if you have a chronic condition, it can be tough to see that 60-day lifetime reserve cap on Medicare Part A hospital coverage. What if you need more care?
How long do you have to stay in a hospital?
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a hospital. Only then will Medicare start to pay for your care in a skilled nursing center for additional treatment, like physical therapy or for regular IV injections. The amount of time you spend in the hospital as well as the skilled nursing center will be counted as part of your hospital benefit period. Furthermore, you are required to have spent 60 days out of each in order to be eligible for another benefit period.#N#However, the portion you are expected to pay for the costs of a skilled nursing center differs from the portion you pay for hospital care. In facilities like these, you must pay in any given benefit period: 1 $0 for your room, bed, food and care for all days up to day 20 2 A daily coinsurance rate of $161 for days 21 through 100 3 All costs starting on day 101
What is Medicare Supplemental Insurance?
As for Medicare supplemental insurance, also known as Medigap, it’s a supplemental policy that you can buy to help offset the costs of Original Medicare.
How much is Medicare coinsurance?
The Medicare recipient is charged a daily coinsurance for any lifetime reserve days used. The standard coinsurance amount is $682 per day. If you’re enrolled in a supplemental Medicare insurance program, also known as “Medigap,” you will receive another 365 days in your lifetime reserve with no additional copayments.
How much is the hospital stay deductible for Medicare?
You will be expected to pay for the initial cost of your hospital stay up to a limit of $1,364. This is your hospital deductible for Medicare Part A. As opposed to other Medicare deductibles, it begins anew with every hospital benefit period, rather than your first admission to the hospital each year. After this deductible is met, Medicare will ...
How long does Medicare last?
Your Medicare benefit period starts the day you are hospitalized as an inpatient and ends once you have been out of the hospital or a skilled nursing facility for 60 days.
How long does Medicare reserve days last?
Medicare offers you 60 lifetime reserve days to extend your Medicare benefit period. Any hospital stays lasting longer than 91 days will require use of lifetime reserve days. These reserve days cost $704 per hospital day in 2020. Medicare only allows you 60 lifetime reserve days total.
How often do you pay a Medicare deductible?
Most health insurance plans have you pay a deductible once a year. With Medicare, you could face multiple Part A deductibles over the course of the year depending on your need for hospital care. It is important to understand that the Medicare benefit period applies to inpatient hospital stays only.
What is the Medicare deductible for 2020?
In 2020, the Part A deductible is $1,408. Any physician fees, however, will be charged to Medicare Part B and are not included as part of the Part A benefit.
How long do you have to be in a skilled nursing facility to be eligible for Medicare?
You also must enter a Medicare-certified skilled nursing facility within 30 days after leaving the hospital. In order for Medicare to pay for care in a skilled nursing facility (SNF), you first have to be hospitalized as an inpatient.
How much will Medicare cut for readmissions?
Any readmissions for these reasons could result in Medicare cutting payments to those hospitals by as much as 3%. 1
When will Medicare Part A start?
on December 14, 2020. Medicare Part A has a benefit period that not only affects how much you will pay for care in the hospital or in a skilled nursing facility (SNF) but how long you will be covered. Unfortunately, understanding how these benefit periods work is not always clear cut.
Do Medicare Benefits Follow the Calendar Year?
Yes, Medicare benefits follow the calendar year since benefits change at the start of each new year.
How Does a Medicare Benefit Period Work?
The Part A Medicare benefit period begins the day of your hospital or skilled nursing facility admission and ends once you’ve been out of the hospital for 60 consecutive days.
How do Medicare Annual Deductibles Work?
The annual deductibles like the Part B or the Part D deductible reset each calendar year. So, you pay the cost of your care first. This is you meet the deductible.
What is a Calendar Year Maximum Out of Pocket?
The maximum out-of-pocket (MOOP) runs on a calendar year. During the calendar year, once you spend a certain amount on covered services, around $9,000, the insurance carrier begins to pick up the rest of your covered medical bills, and you don’t pay any more out-of-pocket.
How To Find Medigap Plans That Cover Your Deductibles
Medicare Supplement insurance can cover the Part A deductible. This way, you don’t have to worry about paying multiple Part A deductibles during the year. Medigap insurance like Plan F or Plan G can leave you with little to no out-of-pocket costs.
When does the benefit period end?
A benefit period under Part A begins the day you’re admitted to the hospital and ends when you’ve been discharged for at least 60 days. If you’ve been out of the hospital for more than 60 days and are admitted again, a new benefit period begins.
How many reserve days are there for Medicare Part A?
Starting on Day 91, you start tapping into your lifetime reserve days for Medicare Part A. You have 60 reserve days. Once they are used up and you encounter a long hospitalization, you are responsible for all costs starting with Day 91 in the hospital.
What is Medicare Part A?
First things first. What is Medicare Part A and what services does it cover?
What would happen if Marge had Medicare Supplement Insurance?
If Marge had a Medicare Supplement Insurance plan, she would have paid $0 in coinsurance for her extended hospital stays.
How to avoid confusion with Medicare Part A?
One way to avoid the confusion associated with Part A’s benefit periods is to enroll in a Medicare Supplement Insurance plan. These private insurance plans help pay for certain out-of-pocket costs associated with Medicare, including the Medicare Part A costs listed above.
How many people are on Medicare in 2019?
Understanding Medicare Part A Benefit Periods. More than 61 million people in the United States received Medicare benefits in 2019, making it a popular and essential health insurance option for seniors and younger people with certain disabilities and medical conditions.1.
What is the most complicated part of Medicare?
One of the most complicated aspects of the federal health insurance program is the benefit periods associated with Medicare Part A (Hospital Insurance).
When does the benefit period end?
The benefit period ends when 60 days have passed since you last received either hospital care or care from a skilled nursing facility.
Why is a benefit period important?
The concept of a benefit period is important because the Medicare Part A deductible is based on the benefit period, rather than a calendar year. With most other types of health insurance (ie, non-Medicare), the deductible is based on the calendar year. Once you meet it, your plan will pay all or part of your costs for the remainder of the year, ...
When does deductible reset for hospitalization?
Once you meet it, your plan will pay all or part of your costs for the remainder of the year, but then your deductible resets on January 1. So if you happen to be hospitalized from December 30 to January 2, you’d have to pay two deductibles with most non-Medicare plans.
How does Medicare benefit period work?
How Do Medicare Benefit Periods Work? It’s important to understand the difference between Medicare’ s benefit period from the calendar year. A benefit period begins the day you’re admitted to the hospital or skilled nursing facility. In this case, it only applies to Medicare Part A and resets ...
How long does Medicare Part A deductible last?
In this case, it only applies to Medicare Part A and resets (ends) after the beneficiary is out of the hospital for 60 consecutive days. There are instances in which you can have multiple benefit periods within a calendar year. This means you’ll end up paying a Part A deductible more than once in 12 months.
What is the deductible for Medicare 2021?
Yearly Medicare Deductibles. The calendar-year deductible is what you must pay before Medicare pays its portion, but you will still have coverage until you reach your deductible. In 2021, the deductible for Part A costs $1,484, while Part B’s deductible is $203.
How long does Medicare cover inpatient care?
Part A covers inpatient hospital care, skilled long-term facility, and more, for up to 90 days. But if you ever need to extend your hospital stay, Medicare will cover 60 additional days, called lifetime reserve days. For instance, if your hospital stay lasts over 120 days, you will have used 30 lifetime reserve days.
How many Medigap plans are there?
One way to avoid paying for deductibles is by purchasing Medicare Supplement, also called a Medigap plan. There are 12 Medigap plans, letters A-N. Each plan varies by price and benefits. All Medigap plans, with the exception of Plan A, cover the Part A deductible.
How many lifetime reserve days can you use?
For instance, if your hospital stay lasts over 120 days, you will have used 30 lifetime reserve days. Please note that you’ll pay a coinsurance of $742 for each lifetime reserve day you use. You can only use your lifetime reserve days once.
How long does a Part A benefit last?
Each benefit period for Part A starts the day you are hospitalized and ends when you are out for 60 days consecutively.
What is a Medicare benefit period?
A benefit period is how Original Medicare measures your use of hospital and SNF services. 1 It begins the day you're admitted as an inpatient in a hospital or SNF and ends when you haven't received any inpatient hospital care (or skilled care in an SNF) for 60 days in a row.
Medicare benefit period and Original Medicare Part A deductible
Unlike other types of health insurance, the deductible for a Medicare benefit period is not based on the calendar year. Instead, you pay a separate deductible for each benefit period—meaning you could pay more than one deductible in the same year.
Medicare benefit period examples
To help you get a better understanding, here are 2 realistic examples:
The bottom line
Knowing how a benefit period works can help you understand your Medicare expenses. To learn more, check out this article on understanding Medicare's out-of-pocket costs.
